Medicare Supplements vs. Medicare Advantage & Prescription Drug Plans
Medicare Supplement/Medigap
It’s recommended that beneficiaries buy a Medicare Supplement/Medigap policy during their 6- month Medigap open enrollment period because, during that time, they can buy any Med Supp policy available for open enrollment that is sold in their state, even if they have health problems. This period automatically starts the month they’re 65 or older and enrolled in Medicare Part B.
Virtually all Medigap carriers permit applications to be submitted three months prior to the beneficiary’s 65th birthday month and/or Part B effective date. Some carriers permit applications to be submitted as early as six months prior to/after said dates with open enrollment considerations.
If a Medicare beneficiary applies for Medicare Supplement coverage after their open enrollment period, they will have to pass medical underwriting unless they’re eligible for guaranteed issue considerations due to a special situation. Virtually all Medigap carriers permit applications to be submitted three months prior to the beneficiary’s 65th birthday month and/or Part B effective date. Some carriers permit applications to be submitted as early as six months prior to/after said dates with open enrollment considerations.
Medicare Advantage/PDP
- To enroll in a Medicare Advantage or PDP plan, the beneficiary is required to have a valid election or enrollment period (separate and distinct from their Med Supp open enrollment).
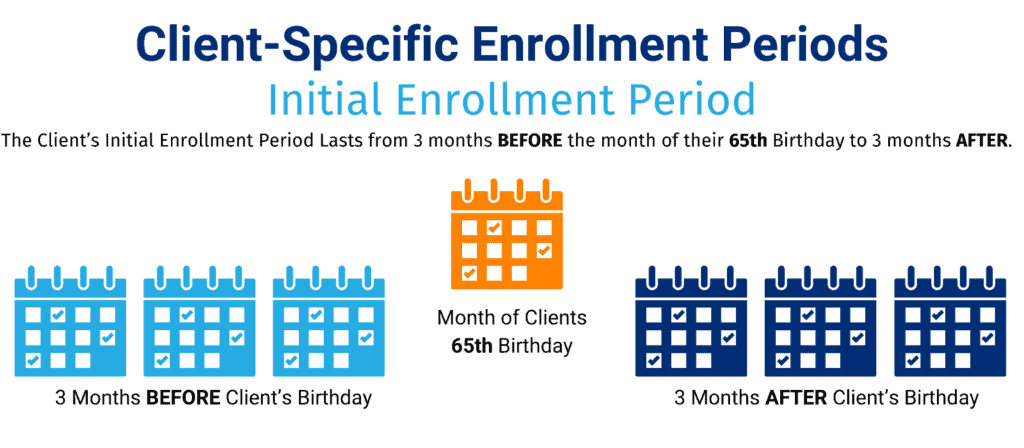
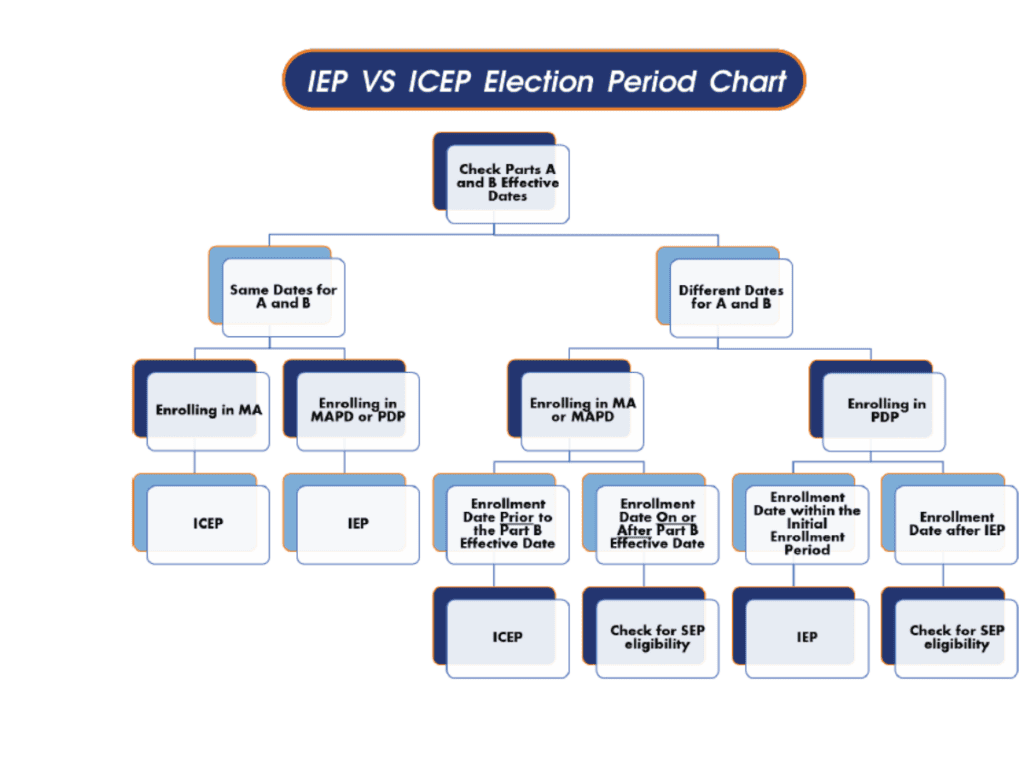
- For beneficiaries that are new to Medicare and have the same Parts A & B effective date, they can enroll in an MAPD or PDP for three months before, the month of, and three months after they turn 65 using IEP. When enrolling before Medicare being in effect, their effective date will be the same as their A & B effective date. When enrolling after Medicare is in effect, their effective date will be the first day of the month following enrollment.
- If they enroll in an MA-only during that time, they can use ICEP. If a beneficiary delays their Part B, they can enroll in an MAPD or MA-only using ICEP. If a beneficiary is enrolling in a PDP past their IEP, they will need to use another election period.
Other Election Periods are Outlined as Follows:
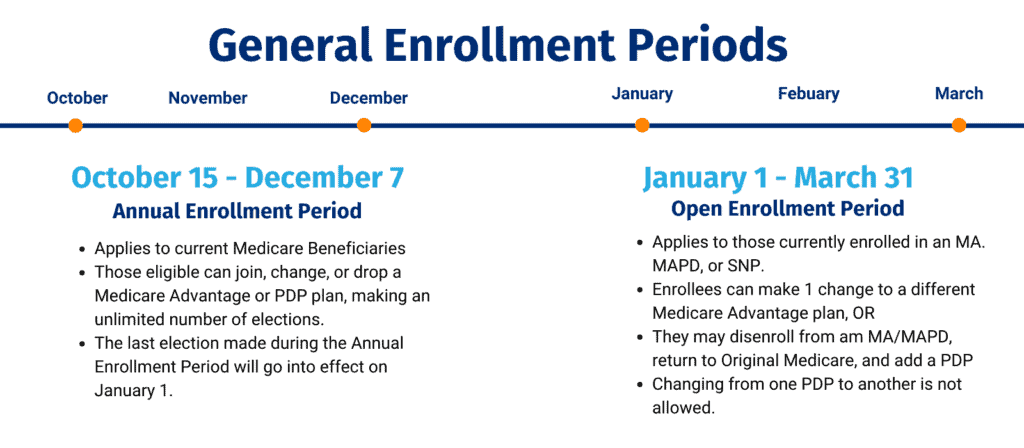
AEP: Annual Enrollment Period
- From October 15 to December 7, any Medicare beneficiary can join, change, or drop a Medicare Advantage or PDP plan. The last election made during that period will go into effect on January 1 of the following year.
OEP: Open Enrollment Period
- From January 1 to March 31, Medicare beneficiaries enrolled in a Medicare Advantage plan (MA/MAPD/SNP) can make one change to a different Medicare Advantage plan or disenroll and return to Original Medicare by enrolling in a PDP. The coverage effective date during OEP will be the first day of the month following the date of their application. The beneficiary cannot change from Original Medicare to Medicare Advantage coverage, nor can they change from one PDP to another PDP using the OEP election.
SEP: Special Enrollment Period
Clients may also enroll and change their coverage outside of the standard enrollment periods if they qualify for a Special Enrollment Period. Coverage obtained during SEP is effective the first day of the month following the date of the application.
Low-Income
- Medicare beneficiaries maintaining their Dual-Eligible or LIS status can add, change, or drop an MA or PDP plan once per calendar quarter for the first three calendar quarters. If a beneficiary gains, loses, or experiences a change in their Dual-Eligible or LIS status, they can make one election during the three months after their change or after they are notified of the change, whichever is later. The coverage effective date for this SEP will be the first day of the month following the date of their application.
Moving
- Medicare beneficiaries who move out of their current plan’s service area, move within their current plan’s service area with new options available to them, or are released from incarceration are granted a SEP. Beneficiaries can make one election from the day they notify the plan in advance of the move to the end of the 2nd full month after the move. Or if they notify their plan after the move, from the day they notify the plan to the end of the 2nd full month after they notify the plan. The coverage effective date for this SEP will be the first day of the month following the date of their application.
FEMA
- From the start of a FEMA-declared emergency or major disaster incident period and for four full calendar months after, Medicare beneficiaries that had a valid election period but did not use it can make one change. The coverage effective date for this SEP will be the first day of the month following the date of their application.
5 Star
- From December 8 to November 30 of the following year, Medicare beneficiaries living in the service area of a 5-star rated plan can make one election to enroll in that plan. The coverage effective date for this SEP will be the first day of the month following the date of their application.

These are not all the Special Election Periods available. The list would be too long to place in this guide. For more guidance around SEP’s reach out to your Sales Development Manager.